Team's member

Project
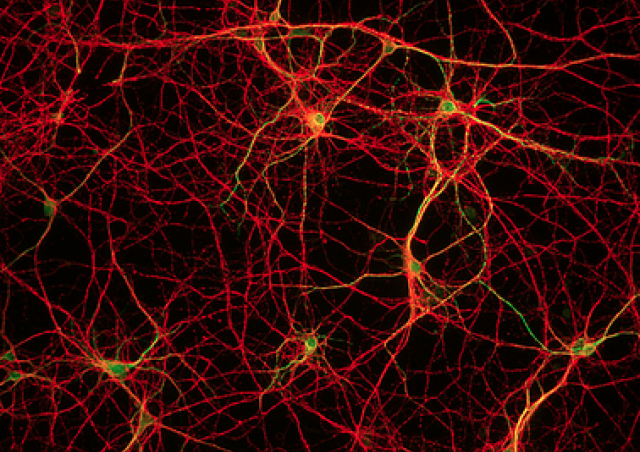
Alveolar macrophages are the most abundant innate immune cells present in the airways that play a crucial role in airway homeostasis. Lung epithelial cells secrete cytokines and express receptors that modulate the activation of alveolar macrophages. This interaction maintains the alveolar macrophage in an anti-inflammatory state at the homeostasis. However, following infection of the epithelium by respiratory viruses such as influenza or human rhinovirus (HRV), although epithelial cells promote activation of the alveolar macrophage, in certain circumstances they can also participate in tissue damage (Villeret et al, 2020) and macrophage dysfunction.
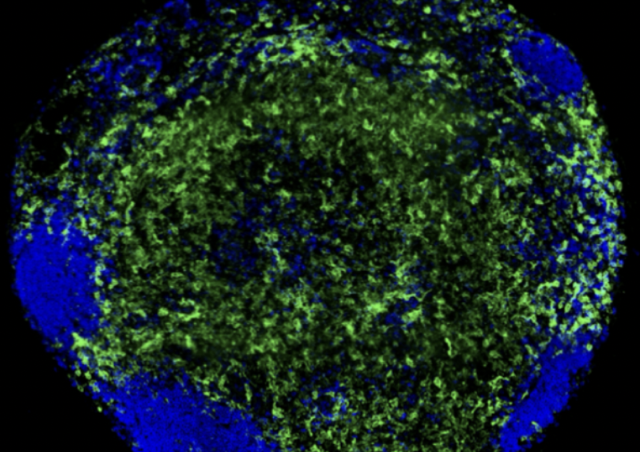
We will use in vitro and in vivo models of influenza (Sanchez-Guzman et al., 2019, Villeret et al., 2018) to study the interactions between infected epithelial cells and alveolar macrophages and to develop new therapeutic strategies that will enhance the alveolar macrophage functions. In particular, we will develop pulmonary influenza vaccine strategies (Sanchez-Guzman et al., 2019, Prince et al., 2023) that will target the respiratory epithelium with suitable adjuvants. The choice of the adjuvant will be important in trying to develop an innate immune memory in the lung, which will enable to establish a more effective immunity against the influenza virus or another infectious agent.
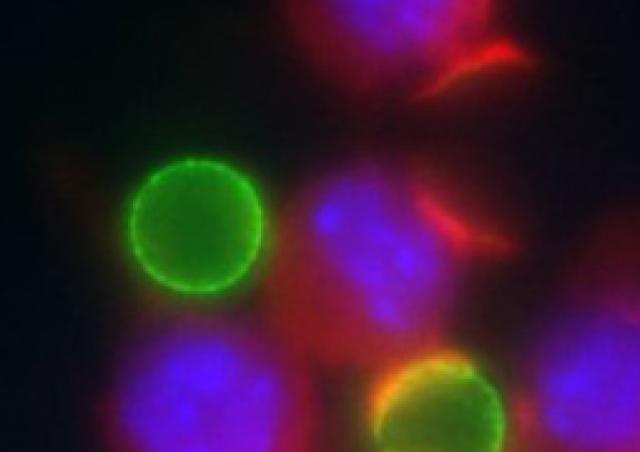
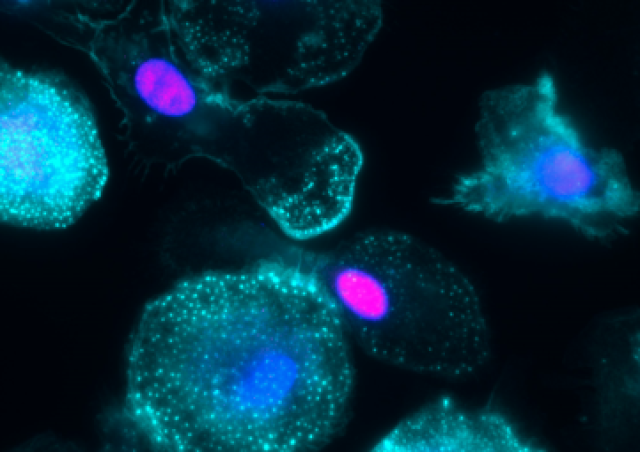
They exhibit defective clearance capacities, often exacerbated by infection with human rhinoviruses (HRV) (Jubrail et al., 2017), in chronic inflammatory diseases such as asthma or chronic obstructive pulmonary disease (COPD). We are dissecting the mechanisms leading to this defective phagocytosis, in collaboration with Astra Zeneca and Prof. Pierre-Regis Burgel (Hôpital Cochin). We monitored the altered cytokine response of macrophages infected by HRV and then challenged with bacterial products (Jubrail et al., 2018) and revealed that Arpin is targeted by human rhinoviruses, explaining the defective bacterial uptake (Jubrail et al., 2020). We showed that the degradative capacity of macrophages and phagosomes maturation are inhibited by HRV in a mechanism dependent of the small GTPase ARL5b (Faure-Dupuy*, Jubrail*, et al., 2024). ARL5b is regulated through the ICAM-1-PKR-1TF2 axis (Faure-Dupuy, et al. 2024). The virus-induced modifications of the phagocytic cells reprogramming are under investigation. A transcriptomic analysis of rhinovirus-treated macrophages allows further identification of new host targets, opening new avenues for potential therapeutic strategies.
References
- Prince, L., Martín-Faivre, L., Villeret, B., Sanchez-Guzman, D., Le Guen, P., Sallenave, J.M., Garcia-Verdugo, I. (2023) Eosinophils Recruited during Pulmonary Vaccination Regulate Mucosal Antibody Production. Am J Respir Cell Mol Biol.68:186-200.
- Villeret, B., Solhonne, B., Straube, M., Lemaire, F., Cazes, A., Garcia-Verdugo, I., Sallenave, J.M. (2020) Influenza A Virus Pre-Infection Exacerbates Pseudomonas aeruginosa-Mediated Lung Damage Through Increased MMP-9 Expression, Decreased Elafin Production and Tissue Resilience. Front Immunol.11:117.
- Sanchez-Guzman, D., Le Guen, P., Villeret, B., Sola, N., Le Borgne, R., Guyard, A., Kemmel, A., Crestani, B., Sallenave, J.M., Garcia-Verdugo, I. (2019). Silver nanoparticle-adjuvanted vaccine protects against lethal influenza infection through inducing BALT and IgA-mediated mucosal immunity. Biomaterials. 217:119308.
- Villeret, B., Dieu ,A., Straube, M., Solhonne, B., Miklavc, P., Hamadi, S., Le Borgne, R., Mailleux, A., Norel, X., Aerts, J., Diallo, D., Rouzet, F., Dietl, P., Sallenave, J.M., Garcia-Verdugo, I. (2018) Silver Nanoparticles Impair Retinoic Acid-Inducible Gene I-Mediated Mitochondrial Antiviral Immunity by Blocking the Autophagic Flux in Lung Epithelial Cells. ACS Nano.12:1188-1202.
- Jubrail, J., Kurian, N., and Niedergang, F. (2017). Macrophage phagocytosis cracking the defect code in COPD. Biomed J 40, 305-312.
- Jubrail, J., Africano-Gomez, K., Herit, F., Baturcam, E., Mayer, G., Cunoosamy, D.M., Kurian, N., and Niedergang, F. (2018). HRV16 impairs macrophages cytokine response to a secondary bacterial trigger. Front. Immunol. 9 :2908.
- Jubrail, J., Africano-Gomez, K., Herit, F., Mularski, A., Bourdoncle, P., Oberg, L., Israelsson, E., Burgel, P.R., Mayer, G., Cunoosamy, D.M., Kurian, N., and Niedergang, F. (2020). Arpin is critical for phagocytosis in macrophages and is targeted by human rhinovirus. EMBO Rep 21, e47963.
- Faure-Dupuy, S.*, Jubrail., J.*, Depierre, M., Africano-Gomez, K., Öber, L., Israelsson, E., Thôrn, K., Delevoye, C., Castellano, F., Herit, F., Guilbert, T., Russell, D.G., Mayer, G., Cunoosamy, D.M., Kurian, N., Niedergang, F. (2024). ARL5b inhibits human rhinovirus 16 propagation and impairs macrophage-mediated bacterial clearance. EMBO Rep. 2024 Mar;25(3):1156-1175.
- Faure-Dupuy, S., Depierre, M., Fremont-Debaene, Z., Herit, F., Niedergang, F. (2024). Human rhinovirus 16 induces an ICAM-1-PKT-ATF2 axis to modulate macrophages functions. J Virol. Oct 22; 98(10):e10149924.