The mucosal-associated immune system is an essential part of the defenses against pathogenic infections. In recent years, our laboratory has identified interleukin 7 (IL-7) as a cytokine produced by mucosae during the first hours following viral infection (Ponte et al. 2017). However, we have also demonstrated that this cytokine stimulates the recruitment of immune cells to the tissues through massive induction of chemokine expression (Beq et al 2009) and could therefore participate in the establishment of mucosal immune responses. The aim of this part of our project is to better understand the mechanisms triggered by local viral replication in the mucosae. We are studying the mechanisms involved in the production of IL-7 in the tissues and its consequences on the physiology of the mucosae. We are also exploring the use of IL-7 as a mucosal vaccine adjuvant able to stimulate the development of strong and prolonged mucosal immunity to allow effective protection at the portals of entry for pathogens into the body.
Project members
Projects
Mechanisms of action of IL-7 in the gut mucosa
Our experiments performed in non-human primate model (Beq et al. 2009; Ponte et al, 2017) have shown that there are cells in the intestinal mucosa capable of responding to IL-7 by producing chemokines. Among the cells of the immune system present in the mucosae, some are known to express the IL-7 receptor (T lymphocytes, antigen-presenting cells) and/or for their ability to produce chemokines. However, many other cell types are involved in the architecture and functioning of the mucosae (epithelial cells, fibroblasts, endothelial cells and smooth muscle cells from the walls of blood and lymphatic vessels). These cells are also described as capable of expressing the IL-7 receptor under certain stimulation conditions, and to participate in the activation of the mucosal immune response (Rancez et al. 2012).
The objectives of this project are to identify the cells of the intestinal mucosa capable of responding to IL-7 and to analyze their contributions to the cell migrations observed in the intestinal mucosa following stimulation by IL-7 in vivo.
IL-7 receptor signaling pathways in stromal cells
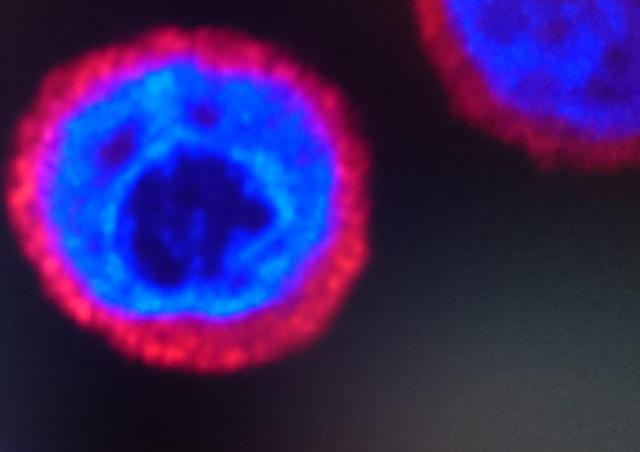
The signal transduction pathway engaged after stimulation of the IL-7 receptor (IL-7R), well described in T lymphocytes, results, via the activation of the JAK/STAT and PI3K pathways, in an increase in metabolism, stimulation of the survival and proliferation of T cells, thus allowing a fine regulation of the homeostasis of these cells. However, the signal transduction pathway induced by IL-7 in stromal cells (epithelial cells, fibroblasts, endothelial and smooth muscle cells of the walls of blood and lymphatic vessels, etc.) of the tissues remains unknown.
This part of the project aims to explore the signal transduction pathways in different types of human and simian stromal cells, in particular endothelial cells and small intestinal fibroblasts. These experiments will be carried out by Western blot, immunohistochemistry on tissue sections and proteomic analysis.
IL-7 as a mucosal vaccination adjuvant
Most viral and bacterial infections are transmitted through the mucosa. However, most vaccines currently being developed mainly target the establishment of systemic immunity. They remain ineffective in inducing strong immunity in the mucosae and in protecting against infection and dissemination of pathogens in the population. The development of a vaccination protocol capable of inducing such immunity is therefore essential and it is necessary, in order to protect human populations against mucosal infections, to develop adjuvants that will allow increasing the mucosal immune response induced by mucosal administration of antigens.
The aim of this part of the project is to develop an original approach to mucosal vaccination, based on the use of the new property of IL-7 demonstrated in the laboratory (Beq et al. 2009). This project aims to exploit the ability of IL-7 to induce, via the stimulation of the local production of chemokines, the massive relocation of immune cells in the mucosae. This property of IL-7 should promote the uptake of mucosally administered antigens, which allows the establishment of a mucosal immune response (Logerot et al 2021). Via the local production of antibodies capable of neutralizing the virus before it penetrates the body, this mucosal immune response should make it possible to block the infection. These studies are carried out in models of viral infections in both mice and non-human primates.
References
Logerot S, Figueiredo-Morgado S, Charmeteau-de-Muylder B, Sandouk A, Drillet-Dangeard AS, Bomsel M, Bourgault-Villada I, Couëdel-Courteille A, Cheynier R, Rancez M. IL-7-Adjuvanted Vaginal Vaccine Elicits Strong Mucosal Immune Responses in Non-Human Primates. Front Immunol. 2021 Feb 25;12:614115. doi: 10.3389/fimmu.2021.614115.
Ponte R., Rancez M., Figueiredo-Morgado S., Dutrieux J., Fabre-Mersseman V., Charmeteau-De Muylder B., Guilbert T., Routy JP., Cheynier R. and Couëdel-Courteille A. (2017) Acute SIV infection triggers early and transient IL-7 production in the gut leading to enhanced local chemokine expression and intestinal immune cell homing. Frontiers in Immunology, 2017 May 19;8:588
Rancez M., Couëdel-Courteille A. and Cheynier R. (2012). Chemokines at mucosal barriers, impact on HIV infection. Cytokine & Growth Factor Reviews. 23(4-5):233-43.
Beq S., Rozlan S., Gautier D., Parker R., Mersseman V., Schilte C., Assouline B., Rancé I., Lavedan P., Morre M. and Cheynier R. (2009). Injection of Glycosylated Recombinant Simian IL-7 Provokes Rapid and Massive T-cell Homing in Rhesus Macaques. Blood, 114 :816-825.