Mucosal Inflammation and Immunity
How does inflammation impact mucosal immunity in the bladder? A balanced inflammatory response is crucial to fight disease while preventing collateral damage. Inflammation drives pathogen clearance, regulates responses to non-infectious disease, and establishes immune memory, whereas inappropriate inflammation induces disease susceptibility or tissue damage. This is especially true in mucosal tissues, which form a critical barrier against the external environment.
The bladder mucosa is highly vulnerable to urinary tract infection (UTI), cancer, and chronic inflammatory diseases of unknown etiology, which all display sex differences in their prevalence. Notably, multidrug resistant uropathogens make up 3 of the top 5 bacteria on the WHO priority list of organisms needing new antibiotics. Thus, in the absence of new non-antibiotic therapies, UTI may go from difficult-to-treat to impossible-to-treat. Bladder cancer is the 5th most common cancer in men and the 11th in women, and is one of the most expensive cancers to treat due to its recurrent nature.
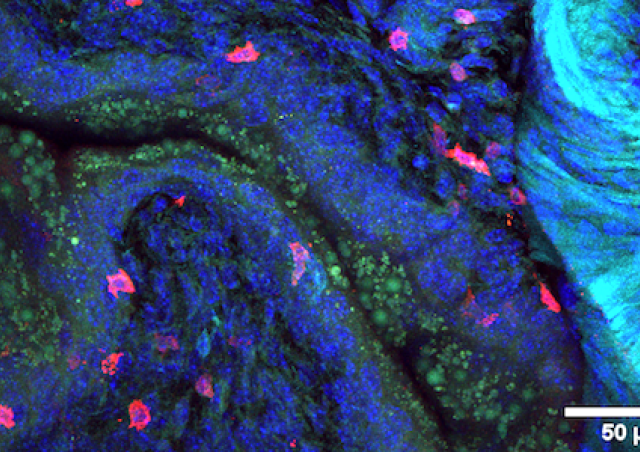
Host-directed immunotherapies may offer new treatment options for bladder diseases. Our work examines innate and adaptive immune responses to UTI and bladder cancer to identify targets for immunomodulation to treat multi-drug resistant UTI and to understand the response to immunotherapies for bladder cancer through fundamental and translational research. We find that a balance of three factors drives “ideal inflammation” in the bladder: the impact of innate immune responses on memory, sex-mediated immune differences, and the bladder microenvironment. Our research projects focus on (1) how innate immune responses shape adaptive immunity, (2) the influence of sex differences on immunity, and (3) (immuno)modulation of the microenvironment to optimize bladder health. Commonalities with other mucosa suggest that our discoveries may extend more broadly to infection or cancer in other mucosal tissues.