Sepsis is a very common disease due to a generalized inflammatory response in reaction to an infection, the most serious form of which, septic shock, remains a frequent cause of death. Despite numerous advances in medicine that reduced this mortality rate, the percentage of sepsis-related deaths remains very high, accounting for 11 million deaths per year worldwide. Patients who survive suffer serious after effects. Due to an aging population, sepsis incidences are expecting to double over the next fifty years. In this context, the search for novel therapeutic avenues is a major public health issue. Endothelial cells, which line blood vessels, are one of the first targets of the inflammatory response linked to sepsis. Endothelial functions are affected, leading to altered vascular tone, barrier function, inflammation and hemostasis. This impairment, referred to as endothelial dysfunction, reduces tissue oxygenation, contributing to the onset of multiple organ failure syndrome. Consequently, many studies have been conducted in recent years to prevent endothelial dysfunction and/or restore endothelial function in order to limit organ failure and improve the prognosis of patients with septic shock. However, to date, no molecule for providing a therapeutic benefit on endothelial dysfunction is available.
To identify effective molecules to prevent endothelial dysfunction, researchers from Institut Cochin, led by Dr. Sandrine Bourdoulous, focused on brain endothelial cells. These specialized cells form a highly restrictive barrier between the blood and the brain (so called the blood-brain barrier) that tightly regulates brain homeostasis and protects the brain parenchyma against systemic infections. The team observed that endothelial cells of cerebral vessels, unlike endothelial cells of peripheral vessels, express intrinsic factors allowing them to resist infection by Neisseria meningitidis (also known as meningococcus). This harmful bacterium is responsible for a very severe form of sepsis, characterized by vascular leakage, disseminated intravascular coagulation, and the appearance of purpuric lesions leading to skin necrosis and death in 30% of patients (purpura fulminans). Among the factors specifically expressed by brain endothelial cells, the researchers identified Angiopoietin-Like 4 (ANGPTL4), and showed that this secreted glycoprotein is a key vascular stabilization factor that protects the blood-brain barrier from bacterial insults.
This work led the researchers to consider using ANGPTL4 as a therapeutic avenue to prevent endothelial dysfunction in sepsis. The team showed, in mouse models of sepsis induced by a bacterial endotoxin or meningococcal-induced purpura, that injection of ANGPTL4 significantly reduced vascular dysfunction and associated symptoms: vascular leakage, intravascular coagulation, production of inflammatory effectors, as well as dysfunction of vital organs such as the lungs and kidneys, and the mortality rate of mice. Finally, the researchers showed that this protection was conferred by a yet uncharacterized domain of ANGPTL4, located in its N-terminal part, through binding to an endothelial receptor, the heparan proteoglycan Syndecan-4.
Considering these very encouraging results, the researchers are continuing their work with a view to clinically using a peptide derived from ANGPTL4 to limit endothelial dysfunction and improve care of patients with septic shock.
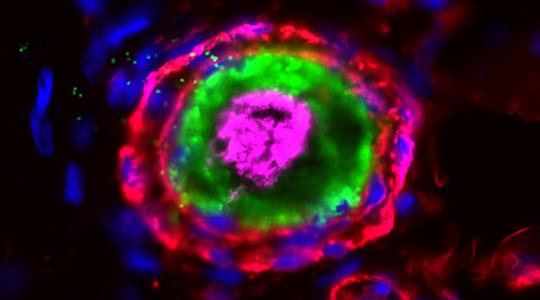
Figure: ANGPTL4 treatment prevents occlusive thrombi formation in Neisseria meningitidis-infected human dermal vessels. Hematoxylin and eosin staining of Neisseria meningitidis-infected human skin. Top: untreated control. Bottom: ANGPTL4-treated.

Reference
Jason Ziveri, Loïc Le Guennec, Isabel dos Santos Souza, Jean-Philipe Barnier, Samuel M. Walter, Youssouf Diallo, Yasmine Smail, Elodie Le Seac’h, Haniaa Bouzinba-Segard, Camille Faure, Philippe C. Morand, Irié Carel, Nicolas Perriere, Taliah Schmitt, Brigitte Izac, Franck Letourneur, Mathieu Coureuil, Thomas Rattei, Xavier Nassif and Sandrine Bourdoulous. Angiopoietin-like 4 protects against endothelial dysfunction during bacterial sepsis. Nature Microbiology. 2024, 10.1038/s41564-024-01760-4.