Endothelial cell response to infection by Neisseria meningitidis
Project leader(s)
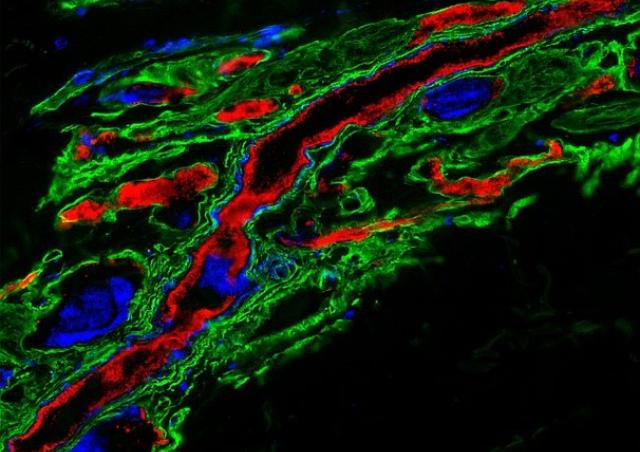
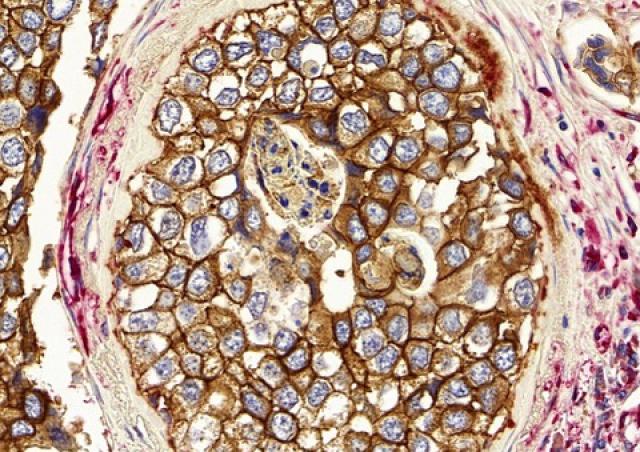
Our team studies the intricate interactions of Neisseria meningitidis (meningococcus) with human peripheral and brain vasculatures, two interactions at the heart of meningococcal pathogenesis (necrotic purpura and meningitis) (1, 2). We are deciphering how N. meningitidis manipulates the endothelial cell response to establish intimate interactions and induce dysfunctions, rupture and breaching of the endothelial barriers (3, 4). We have identified key host and bacterial factors involved in such interactions (5-9) (Patent WO 2014/016152 A1). In addition, we have identified compounds that target type IV pili, reduce vascular colonization by meningococci and prevent subsequent vascular dysfunctions, intravascular coagulation and overwhelming inflammation (10) (Patents WO/2017/121755; WO/2018/083314). Taking advantage of an in vivo model of meningococcal infection, we aim at deciphering the molecular and cellular events leading to vascular dysfunction, thrombosis, organ failure and immune escape by this bacterial pathogen.
At the CNS level, brain microvascular endothelial cells form the blood-brain barrier (BBB), a highly specialized structural and biochemical barrier that preserves brain homeostasis. Our team has engineered a unique human brain endothelial cell line (hCMEC/D3) that phenocopies the normal human BBB, as judged for low permeability, polarized secretion and transport, architectural organization, and protein expression profile (11, 12) [Patent WO/2006/056879, now distributed in more than 300 laboratories worldwide and under license with several pharmaceutical companies]. Taking advantage of this in vitro model, we aim at elucidating the molecular strategies selected by Neisseria meningitidis to colonize human brain vasculature and get access to the brain with a minimal loss of BBB integrity (13). Our objectives are to identify the potential protection mechanisms of the brain from local vascular damages due to bacterial infections, with the ultimate objective to implement endothelial protection mechanisms to limit the detrimental haemostatic and inflammatory processes associated to invasive meningococcal diseases.
1. (Coureuil et al., 2014) 2. (Coureuil et al., 2017) 3. (Lemichez et al., 2010) 4. (Coureuil et al., 2013) 5. (Coureuil et al., 2010) 6. (Bernard et al., 2014) 7. (Maissa et al., 2017) 8. (Le Guennec et al., 2020) 9. (Dos Santos Souza et al., 2020) 10. (Denis et al., 2019) 11. (Weksler et al., 2005). 12. (Weksler et al., 2013) 13. (Le Guennec et al., 2020).