Project members
Projects
Colorectal cancer (CRC) and hepatocellular carcinoma (HCC) are the two leading causes of death among solid cancers of the gastrointestinal tract. In recent years, chemotherapy or immune checkpoint inhibitors (ICI) have revolutionized the therapeutic management of patients with advanced CRC and HCC. However, less than half of these patients respond sustainably to these treatments due to primary or adaptive resistance mechanisms. Alterations in the energy metabolism of cancer and immune cells are often associated with these resistance mechanisms.
The activity of our team thus aims to understand the mechanisms by which alterations in the energy metabolism within the tumor contribute to the progression of CRC and HCC, to the escape of immune control and to resistance to treatments in preclinical models. Thanks to collaborations between researchers and clinicians from the Cochin Institute, our ambition is to transfer our fundamental discoveries to the clinic with the aim of identifying new biomarkers making it possible to offer treatments adapted to patients and to be able to identify new therapeutic strategies.
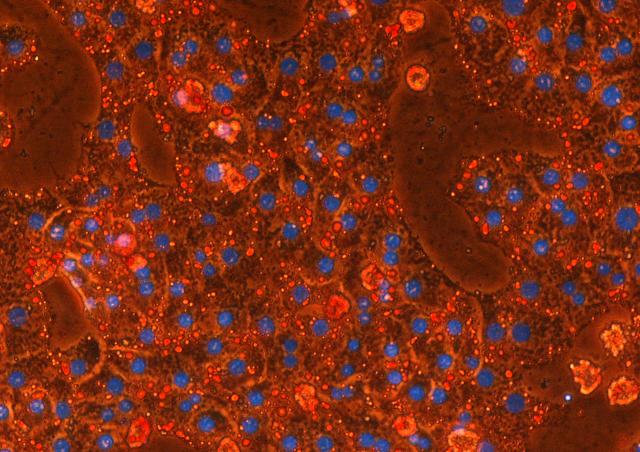
Our team brings together expertise and unique tools from fundamental and clinical research to characterize the molecular mechanisms of adaptive responses of cancer cells to therapies. Through complementary approaches such as metabolomics, isotope profiling techniques, transcriptomics, culture of 3D organoids and the development of mathematical models, our aim is to characterize the nature of deregulated metabolic networks in cancer in order to determine whether their pharmacological targeting may contribute to the development of new treatment strategies.
Scientific project
Despite the extraordinary progress made in recent years in treating cancer, there is still no comprehensive approach to prevent the development and recurrence of cancers of all types. The mission of our team at the Cochin Institute is to better understand the molecular and cellular mechanisms underlying several cancers, in the hope that this knowledge will lead to the development of new therapeutic approaches. Our research thus contributes in particular to the fight against two widespread cancers with a poor prognosis, colorectal cancer (CRC) and hepatocellular carcinoma (HCC).
Our team can provide its expertise in the characterization of the different components of cell metabolism.
Targets
- Glycolysis
- Mitochondrial metabolism
- Amino acids synthesis
- Lipid Synthesis and use
Innovative technologies
- Metabolomics and isotope profiling (13C) and metabolic flux (14C)
- Characterization of cellular metabolism (Seahorse, measurement of cellular respiration (OROBOROS), assay of enzymatic activity and redox status, etc.)
- Development of organoids of CRC and CHC.
- Development of new genetic models of CRC and CHC.
- Genetic (CRISPR / CAS9) and pharmacological screening
Current projects
Axis 1: Metabolic reprogramming and cancer
- Colorectal cancer (CRC)
This study aims to identify the best strategies to prevent the development of colorectal cancer. Our main objective is to determine whether targeting the energy metabolism of the tumor represents a new therapeutic perspective for cancer treatments. The team is studying how the reprogramming of the oxidative metabolism of the cancer cell participates in the development of CRC, by focusing on the function of the mitochondrial protein UCP2 (uncoupling protein 2) and this with respect to the immune response, cell proliferation and colonic carcinogenesis process. Our team has shown that UCP2 participates in the reprogramming of cell metabolism, in particular the oxidation of glucose and fatty acids, in different cell models. We have demonstrated that cancer cells overexpressing UCP2 alter their metabolism from glycolysis to oxidative phosphorylation and become less tumorigenic (Esteves et al., 2014). Moreover, its overall loss promotes tumor development in CRC mouse models (Aguilar et al., 2019). Indeed, the metabolic reprogramming induced by the loss of UCP2 increases oxidative stress and promotes the development of CRC. We are also studying whether this metabolic modulation also modulate the immune response. Thus, UCP2 appears to be an excellent target for linking metabolism, redox balance and immune response, which are intimately involved in the development of CRC.
- Hepatocellular carcinoma (HCC)
In humans, the initiation and development of HCC are particularly correlated with the increase in the number of patients with metabolic syndrome (obesity, diabetes, hepatic steatosis). Due to its central role in the control of carbohydrate and lipid metabolism in the liver, we hypothesized that the glucose-sensitive transcription factor ChREBP (Carbohydrate Responsive Element Binding Protein) could play a key role in the initiation and development stages of HCC. We show for the first time in mice that an increase in the transactivating activity of ChREBP in the hepatocyte is sufficient by itself to initiate the development of a poor prognosis HCC (Benichou et al., In review). Molecularly, ChREBP exerts its pro-proliferative and pro-oncogenic effects on the hepatocyte by stimulating the activity of the PI3K / AKT signaling pathway. In addition, the increased activity of ChREBP reroutes glucose and glutamine metabolism metabolic fluxes towards anabolic pathways to sustain de novo lipids and nucleotides biosynthesis necessary for tumor cell proliferation and tumor growth. Thus, ChREBP constitutes a therapeutic target of choice for the development of new treatment strategies for HCC.
Axis 2: Metabolism and tumor immunity
Over the past two decades, advances in onco-immunology have led to the development of various forms of immunotherapies that mobilize the immune system to promote or restore an effective anti-tumor immune response. While it is well accepted that the immune system plays an essential role in monitoring the emergence of malignant cells (concept of immunosurveillance), its immunosuppressive functions and its contribution to the tumorigenesis process associated with the progression of the disease and resistance to treatment remain less well defined. Although unprecedented improvements in tumor control have been achieved with therapeutic monoclonal antibodies that release inhibitory checkpoints of the immune system, such as antibodies blocking the PD-1 / PD-L1 axis, it is now evident that only a minority of patients receiving this type of immunotherapy respond to treatment, and native or acquired resistance to these inhibitors is common. Many efforts are therefore currently being made to identify new targets which activate, trigger or improve anti-tumor immune responses.
In this context, a better understanding of the relationships between energy metabolism, cancer cells and cells of the immune system is essential in order to optimize current treatments. Through an in-depth analysis of the tumor microenvironment, our team, in close collaboration with clinicians, is working to decipher the molecular and cellular immunosuppressive mechanisms. Our team is particularly interested in the role of metabolism in lymphocytes and macrophages in tumor development and anticancer treatments.
In CRC and HCC, our projects aim to 1/ characterize the tumor immune microenvironment associated with tumor progression and resistance to treatment 2/ identify new metabolic strategies blocking immunosuppressive mechanisms that contribute to the escape of tumor cells from immune surveillance 3/ provide proof of concept for these new therapeutic strategies in preclinical and clinical models. Our long-term objectives are to identify new therapeutic targets and to provide proof of the concept of new metabolic strategies to improve the response to immunotherapy treatments.