Members of the project
Introduction
Regulatory T cells (Treg cells) are the main mediators of peripheral tolerance under physiological settings. In the periphery, Treg cells encompass cells that have been naturally produced within the thymus, called thymic Treg cells (tTreg cells), and cells with similar phenotype and functions that have differentiated from naïve CD4 T cells following antigen recognition in secondary lymphoid organs, called peripheral Treg cells (pTreg cells).
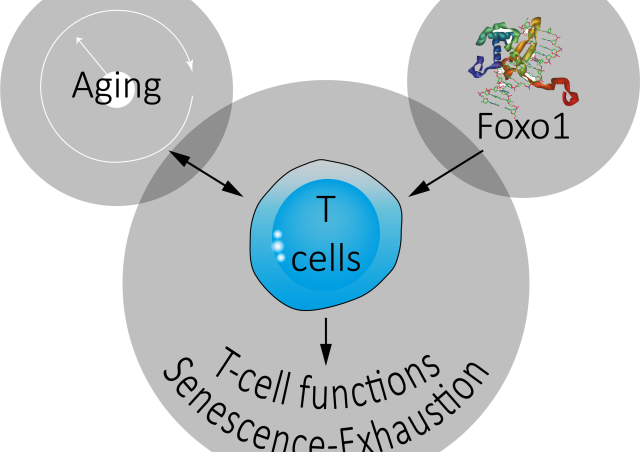
Although they share a similar phenotype (characterized in particular by the expression of the transcription factor Foxp3) and equivalent functions, tTregs and pTregs are only partially redundant in inhibiting immune responses. The complementary role of tTreg and pTreg cells, demonstrated for instance in the prevention of autoimmune diseases could be explained in part by their distinct TCR repertoires. Indeed, whereas tTreg cells, generated in response to interactions with the Self (Self peptide complex - Self major histocompatibility complex (MHC)) during their selection in the thymic medulla, display a repertoire biased towards the Self, that of pTreg cells is potentially broader. Importantly, the mechanisms underlying the generation of these 2 subpopulations of Treg cells also differ. Indeed, in contrast to tTreg cells, the emergence of pTreg cells from naïve CD4 T cells is controlled by TGFβ. TGFβ signaling pathways and response elements within the Foxp3 gene (CNS1) thus drive pTregs differentiation without affecting tTregs generation.
While defects in the development of thymic Tregs lead to immune dysregulation and life-threatening systemic autoimmune manifestations, the role of pTregs has so far only been demonstrated in the prevention of inflammation of the intestine or lung mucosa and in fetomaternal tolerance. It remains to be determined whether pTregs participate in immune regulation in other homeostatic or pathological contexts.
Aim #1
Deciphering the TGFβ-dependent signaling pathways leading to the generation of peripheral regulatory T cells
While TCR and IL-2 signaling pathways dictate tTreg cell generation from thymic precursors (preTreg cells), TGFβ signaling is crucial for the differentiation of naïve CD4 T cells into pTreg cells in vitro and in vivo. TGFβ binds to a hetero-tetrameric receptor complex composed of TβRI and TβRII that triggers the canonical SMAD pathway as well as numerous other signaling modalities, including MAPK, AP-1, PI3K and NFκB pathways. In the canonical SMAD pathway, SMAD2 or SMAD3 (SMAD2/3), phosphorylated by TβRI, form a complex with SMAD4 and translocate into the nucleus for transcriptional regulation. Foxp3 gene expression is controlled by a core promoter and at least 4 enhancers (conserved noncoding sequences, CNS0 and 1-3). Each regulatory element contains a variety of transcription factor binding sites which regulate foxp3 promoter activity. CNS1 is located between exons -2b and -1 of the Foxp3 gene and besides transcription factor binding sites for Rel-NFAT, CREB, RAR/RXR and AP-1 harbors a consensus sequence for Smad3. Consistently, mice with a targeted deletion of the Foxp3 CNS1 enhancer (CNS1KO mice), or deficient for Smad4 (Smad4KO) or Smad2 and Smad3 (Smad2/3DKO) have an impaired commitment of naive T cells to the pTreg cell lineage in vitro.
However, this impaired ability of naïve CD4 T cells from Smad4KO, Smad2/3DKO or CNS1KO mice to commit into pTreg cells is only partial. Indeed, in vitro Treg cell polarization assays in response to TGFβ reveal a 50% decrease in the proportion of Foxp3-expressing cells arising from naïve CD4 T cells from KO mice when compared with WT mice. Altogether, these results suggest that half of the TGFβ dependent conversion of naïve CD4 T cells into Treg cells is Smad- and CNS1-independent.
Using newly generated deficient mice, we now plan to decipher TGFβ-dependent Smad-independent signaling pathways leading to pTreg cell generation in vitro and in vivo.

Aim #2
Contribution of peripheral and thymic regulatory T cells in the suppression of anti-tumor immune responses
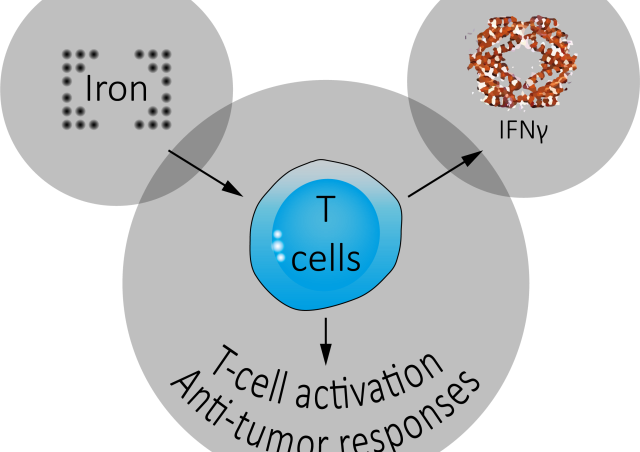
Both development and progression of cancer are influenced by factors outside the tumor cells. Among these, the immune system plays a major role in enhancing or inhibiting tumor progression. T lymphocytes are perfect examples of this duality. Indeed, CD4 or CD8 effector T cells producing IFNɣ are powerful anti-tumor actors while regulatory CD4 T cells (Treg cells) expressing the transcription factor Foxp3 are crucial actors in the inhibition of anti-tumor immune responses.
While Treg cells have been the target of numerous studies, especially in the tumor context, it is surprising to note that the relative contribution of pTreg versus tTreg cells to tumor progression remains under-studied. We therefore propose to determine the contribution of pTregs to the suppression of anti-tumor immune response by evaluating the respective roles of both Treg cell subsets in the inhibition of anti-tumor responses using, among other tools, genetically-modified mouse models.